Perioperative Cardiovascular Management for Noncardiac Surgery: An African Perspective
Eileen Stuart-Shor, PHD, Janet Dewan, PHD, CRNA, Aaron Sonah, RNA, Huma Syed Hussain, MD
Published April 18, 2025 | Clinics in Medical Education
Issue 6 | Volume 1 | April 2025
Each month, the Boston Africa Anesthesia Collaborative (BAAC) hosts grand rounds to facilitate case-based learning and knowledge exchange in anesthesia practice across resource-limited settings in Liberia. The January session featured a focused discussion on Perioperative Cardiovascular Management for Noncardiac Surgery: An African Perspective.
Perioperative cardiac complications account for one-third of all perioperative deaths. Despite this significant burden, there is a lack of robust, evidence-based guidelines for perioperative cardiovascular risk stratification and management of cardiac patients undergoing noncardiac surgery in low- and middle-income countries (LMICs). International guidelines typically determine preoperative cardiovascular risk based on demographic variables (e.g., age), cardiovascular risk factors (e.g., comorbidities), and surgical risk (e.g., intermediate- to high-risk surgery). However, these guidelines may not fully address the unique challenges and resource limitations present in the African context.
The African Surgical Outcomes Study (ASOS) trial provided critical data on perioperative risk in African settings, assessing tools such as the Duke Activity Status Index and frailty scores for preoperative evaluation. These assessments help understand functional capacity and frailty, which are essential for perioperative risk stratification in resource-constrained environments.
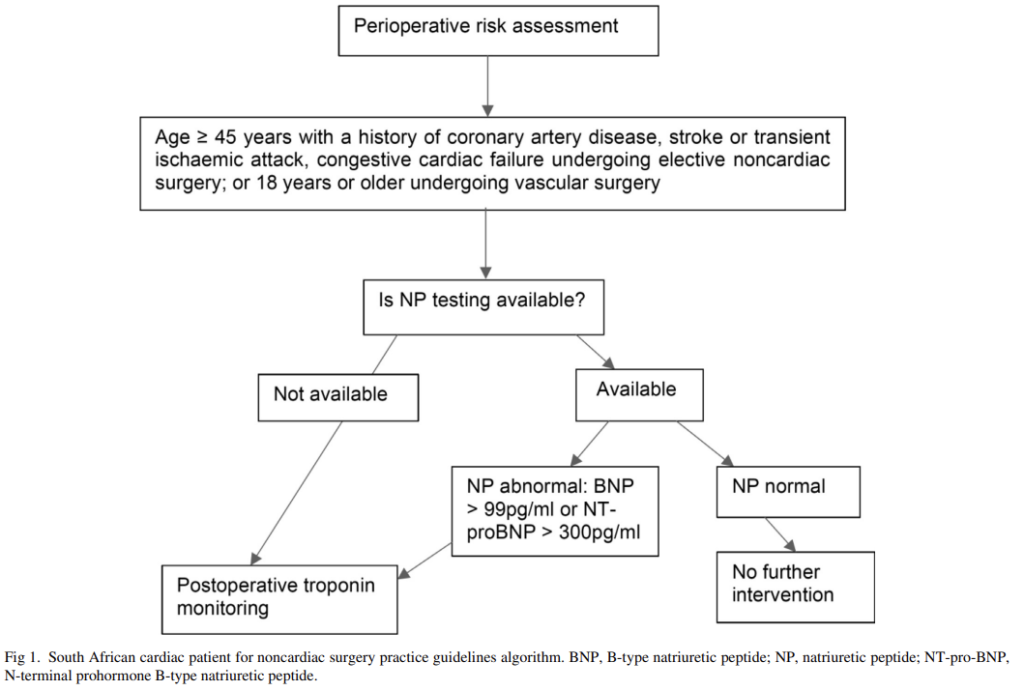
The South African guidelines for the cardiac patient undergoing noncardiac surgery were developed to provide relevant recommendations for Africa. These guidelines were based on an adaptation of the Canadian Cardiovascular Society Guidelines, incorporating literature from African countries and recent research. The recommendations were refined through a Delphi consensus process involving South African anesthesiology and vascular surgery experts.

Key Recommendations:
1. Preoperative Risk Stratification: Elective noncardiac surgical patients aged ≥45 years with a history of coronary artery disease, congestive heart failure, stroke, or transient ischemic attack, as well as vascular surgery patients aged ≥18 years with peripheral vascular disease, require further preoperative risk stratification. Their predicted 30-day major adverse cardiac event (MACE) risk exceeds 5%. This recommendation aligns with international guidelines and remains relevant in both African and U.S. contexts.
2. Non-invasive Cardiovascular Testing: Routine non-invasive cardiovascular testing before elective noncardiac surgery is not recommended. In the U.S., a baseline electrocardiogram (ECG) is commonly performed for postoperative comparison. However, in many African settings, unnecessary testing is avoided due to financial constraints. ECGs are only conducted when indicated by symptoms or a history of heart failure or stroke, as highlighted by a Liberian healthcare professional.
3. Preoperative Natriuretic Peptide (NP) Screening: Preoperative NP screening is recommended for elective noncardiac surgical patients aged ≥45 years with a history of coronary artery disease, stroke, transient ischemic attack, or congestive heart failure, and for vascular surgical patients aged ≥18 years with peripheral vascular disease. Despite strong evidence supporting this recommendation, its implementation is limited in some African countries due to the unavailability of NP testing in smaller clinics, as noted by Liberian healthcare professionals. Despite strong evidence supporting this recommendation, its implementation is limited in some African countries due to the unavailability of NP testing in smaller clinics, as noted by Liberian healthcare professionals.
4. Postoperative Troponin Monitoring: Daily postoperative troponin measurements for 48–72 hours are recommended for high-risk noncardiac surgical patients, specifically: i) Patients with a baseline MACE risk >5% at 30 days post-surgery (if no preoperative NP screening was performed). ii) Patients with elevated preoperative BNP (>99 pg/ml) or NT-proBNP (>300 pg/ml).
This guideline is designed to detect myocardial injury following surgery. A Liberian healthcare worker emphasized that troponin testing is already used in their setting to diagnose and monitor heart failure severity and predict future cardiovascular complications.
While the South African guidelines offer a structured approach, their applicability varies across African nations due to differences in healthcare infrastructure and resource availability. The Liberian medical team highlighted that healthcare systems across Africa are heterogeneous, and a one-size-fits-all approach may not be feasible. Local adaptations of perioperative cardiovascular guidelines must consider the specific healthcare realities of each country, balancing evidence-based recommendations with practical feasibility.
Perioperative cardiovascular management for noncardiac surgery in Africa requires context-specific guidelines that acknowledge resource limitations and healthcare disparities. While international frameworks provide a foundation, African healthcare systems must tailor recommendations based on available resources and local expertise. Collaborative efforts are crucial to improving perioperative outcomes and reducing cardiac complications in surgical patients across the continent.
REFERENCES
1. Thompson, Annemarie et al. “2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM Guideline for Perioperative Cardiovascular Management for Noncardiac Surgery: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines.” Circulation vol. 150,19 (2024): e351-e442.
