A Bioethics and Professionalism Curriculum Framework for Anesthesiology Training Programs – PART TWO
Shahla Siddiqui, MD, Altan Marvi
Published October 1, 2024 | Clinics in Medical Education
Issue 3 | Volume 1 | September 2024
Goals of Ethics and Professionalism Curricula
Although medical ethics and professionalism teaching may be done in differing ways, there is a need for more standardization in the curriculum and in evaluation and long-term outcome assessment. It is suggested in literature that a well-designed curriculum not only enhances the learning experience but also ensures that learners acquire the necessary knowledge and skills in a structured and efficient manner.1 Making ethical competence learning possible, as well as having emotional awareness of one’s own thoughts, biases and perceptions, and upholding a patient’s best interests and autonomy are important aspects when seeking to increase the understanding and management of ethical problems in everyday clinical work. It has been suggested that through rigorous ethical teaching, debate and discussion of clinical contexts in an interdisciplinary manner, the focus of such a curriculum should be expansion of ‘cognitive knowledge, behavioral skills, and development of a professional character.’1
In a review of ethics curricula and needs assessment, there was a preponderance of ethical topics related to a patient’s right to self-determination.1
1. In designing a curriculum, the initial key points to consider should be as outlined in the table below:
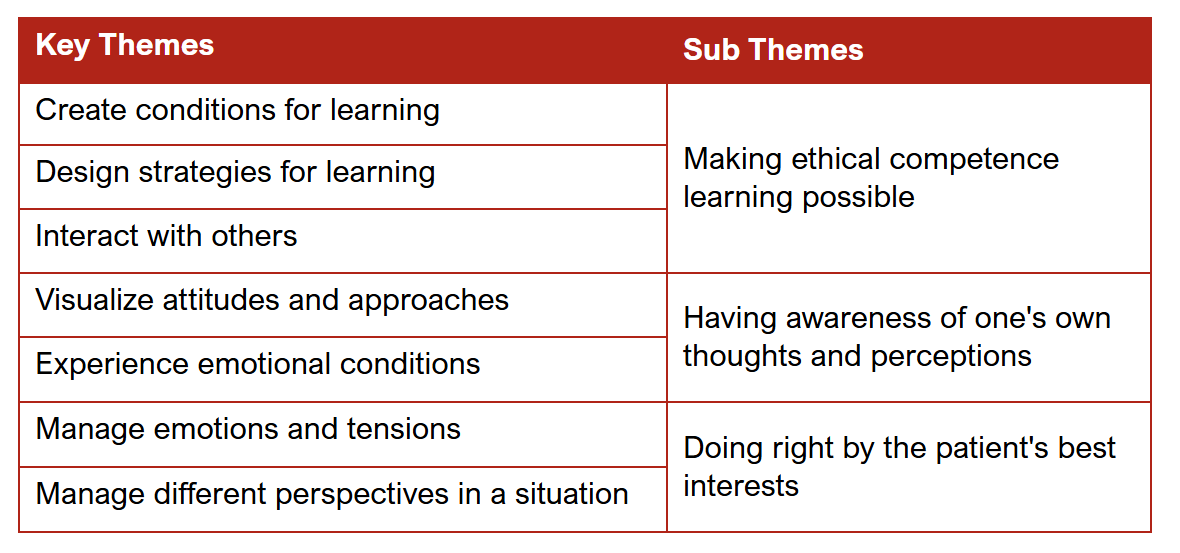
TABLE 1
Curriculum themes
Broad Objectives
Step 1: Define clear objectives,
Step 2: Conduct a needs assessment: survey residents, fellows, nursing, patients and faculty,
Step 3: Organize content systematically, and involve other fields such as ethics, social work and nursing,
Step 4: Choose appropriate instructional methods: lectures, case discussions, role play, debate, journal club, simulation,
Step 5: Develop assessment strategies: such as OSCE or role play,
Step 6: Integrate innovation and technology, such as virtual reality, and artificial intelligence if possible.1
2. Secondly, the content included should be carefully considered and based on evidence in literature as well as local requirements, such as hospital culture, state and federal laws and cross-cultural considerations. Such an integrative systematic review by Pence et al, provides insights into ethics education for healthcare professionals, students, and educators. The results show that ethical competence learning is essential when seeking to draw attention to and deal effectively with ethical problems.
Healthcare professionals and students in clinical practice need a supportive learning environment in which they can experience a conducive climate for reflection on ethical challenges, conflicts, or dilemmas that influence everyday healthcare work. The design and course content of ethics education meant to increase the understanding and management of ethical problems in clinical practice should be interdisciplinary and interactive. Input from supportive teams such as nursing and social work would be vital in the success of such education.1
Prior studies have identified certain areas to focus on but they need to be validated in the local setting. In the perioperative scenario, the topics that could commonly be experienced include, but are not limited to (Table 2):
Among programs in medical ethics and professionalism, the Harvard Medical School program offers a holistic curriculum focused on Equity and Anti-Racism, Professionalism, Cultural Humility and Structural Competence, Community Engagement and Learning, Advocacy and Activism, as well as Interprofessional Education.
In addition, among the pedagogy theories is the Learning Triangle1 which represents the ‘self-organizing process that occurs when individuals bring together their theoretical knowledge and challenges with their practical knowledge and challenges to produce new learning.’ This interplay of learner, teacher and knowledge can produce an interactive progression from novice to expert and with a goal to create a respectful, reciprocal, reflective dialogue on teaching and learning.
3. Tools for teaching could include the following proven interactive interprofessional education (IPE) methods: Lectures, debates, simulations, roleplay etc.
4. Tools for assessment of milestones achieved will need to adhere to current standards of ACGME and departmental requirements. Longitudinal assessment and 360-degree appraisals from teams and patients would also be counted.
Conclusion
Further studies on ethics education are needed. Comparative research, through which different educational designs can illuminate what provides the best possible learning process for managing ethical problems, would be valuable. Intervention studies aiming to maintain and protect the autonomy of patients with impaired decision-making capabilities may also be warranted. Another interesting area for further study is about the educators and their competencies in ethics education, with a special focus on the requirements for such competence. Further research could be used to develop healthcare professionals’ and students’ readiness and capabilities to recognize and respond appropriately when they encounter ethically problematic situations. This would, in turn, give healthcare professionals and students a sense of self-confidence in their everyday clinical practice.
REFERENCES
1. Boudjeltia KZ, Lelubre C. Relations entre la pensée scientifique et la médecine: les apports de Platon et d’Aristote [Relations between the scientific thought and the medicine: the contributions of Plato and Aristotle]. Rev Med Brux. 2015 Jan-Feb.
2. Accogli A, Vergano M. Managing the Labyrinth of Complex Ethical Issues in Anesthesia Practice: The Anesthesiologist’s Ariadne’s Thread. Anesthesiol Clin. 2024 Sep.
3. Mahajan A, Esper SA, Cole DJ, Fleisher LA. Anesthesiologists’ Role in Value-based Perioperative Care and Healthcare Transformation. Anesthesiology. 2021 Apr.
4. Evers AS, Wiener-Kronish JP. Roles for Anesthesiologists in the Future of Medicine in the United States. Anesth Analg. 2022 Feb.
5. Conran RM, Powell SZ, Domen RE, McCloskey CB, Brissette MD, Cohen DA, Dixon LR, George MR, Gratzinger DA, Post MD, Roberts CA, Rojiani AM, Timmons CF Jr, Johnson K, Hoffman RD. Development of Professionalism in Graduate Medical Education: A Case-Based Educational Approach From the College of American Pathologists’ Graduate Medical Education Committee. Acad Pathol. 2018 Jun.
6. Pence MJ, Pla RA, Heinz E, Douglas R, Shaykhinurov E, Jacobs B. Identifying Relevant Topics for Inclusion in an Ethics Curriculum for Anesthesiology Trainees: A Survey of Practitioners in the Field. Camb Q Healthc Ethics. 2024 Apr.
7. Ludmerer KM. Instilling professionalism in medical education. JAMA. 1999;282(9):881-882.
8. Lo B, Schroeder SA. Frequency of ethical dilemmas in a medical inpatient service. Arch Intern Med. 1981;141(8):1062-1064.
