Crack the Code: How Problem-Based Learning Transforms Education
Matthew Gao, MD, John Bellamente, MD
Published September 5, 2024 | Clinics in Medical Education
Issue 2 | Volume 1 | August 2024
As part of the Education Scholarly Program, “Train the Trainers”, Drs Matthew Gao and John Bellamente anesthesiologists at BIDMC Anesthesia, Critical Care and Pain Medicine delivered a presentation to introduce Problem Based Learning (PBLs) and their approach to incorporate PBL into anesthesiology education. With the widespread use of internet-based services, new approaches to post-graduate medical education are becoming available. In PBL, learners are challenged with a real-world problem and concepts are introduced as the solution takes shape. Through this form of active learning, several educational objectives can be achieved compared to more traditional teaching methods, i.e. lecture-based learning (see table 1). Since PBL is learner-centered, the role of the teacher is that of a moderator/facilitator to direct the learning process. In these sessions, teachers tailor discussions in a welcoming environment to encourage learners to raise questions and explore ideas. Learners can then investigate, collaborate, build on prior knowledge, and become motivated for self-directed learning at each session’s end. Teachers play a crucial role in PBL, so proper training is paramount to a successful session.

Table 1
Teaching methods, their descriptions, and how likely they are to meet educational objectives. 1 = unlikely to meet, 5 = very likely to meet. SCC: structured clinical context; CRP: clinical reasoning process; SDL: self-directed learning; MOT: motivation for learning.
The role of faculty in PBL is pivotal, serving as facilitators rather than traditional instructors. Faculty members guide students through the problem-solving process by providing support, posing probing questions, and helping them navigate complex clinical issues without directly supplying answers.
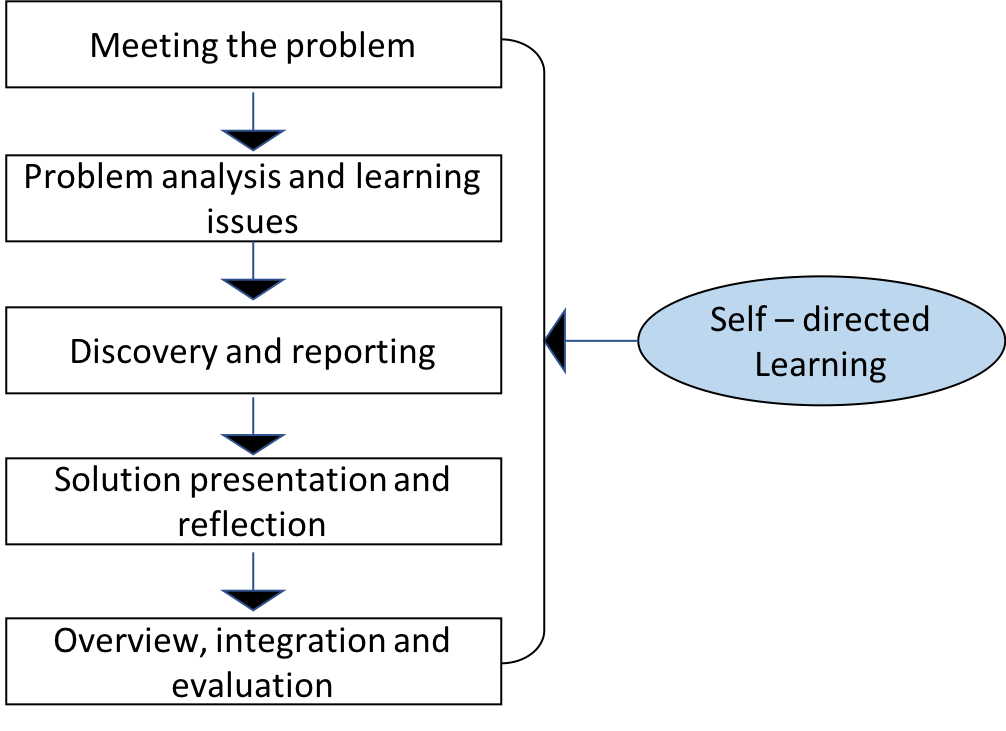
Figure 1
Process of PBL
