Optimization of Adductor Canal Block for Lower Extremity Anesthesia: Evidence-Based Approaches
Federico Puerta Martinez, MD, Victor Polshin, MD
Published December 2, 2024 | Clinics in Medical Education
Issue 4 | Volume 1 | November 2024
John Smith is a 42-year-old male working as a construction worker who presented with severe knee pain following a fall at work. He reported slipping and landing directly on his right knee, experiencing immediate pain, swelling, and an inability to bear weight or extend the knee.
Upon examination in the emergency room, there was noticeable swelling, bruis- ing, and deformity over the knee. The patient had no active extension of the knee, and passive motion was limited due to pain. Strength testing showed that he was unable to perform a straight-leg raise, though distal pulses and sensation were intact on neurovascular examination. Imaging revealed a transverse patellar fracture with 3-4 mm of displacement, along with an associated extensor mechanism disruption. In terms of regional blocks what options do we have?

Figure 1
Imaging shows a transverse patellar fracture.
Anatomy
In this case of a patellar fracture, the focus is on the innervation of the anterior knee, particularly the patella and surrounding structures. Key contributors to the anterior knee’s innervation include the following branches of the femoral nerve (FN) (1) Nerve to Vastus Medialis: (supero-medial aspect of the patella), (2) Nerve to Vastus Lateralis: (lateral aspect of the patella) and for this particular case the (3) Sephanous nerve (Infrapatellar Branch). The saphenous nerve is a branch of the posterior division of the femoral nerve and it is purely a sensory nerve. It leaves the femoral triangle and passes through the adductor canal (sub-sartorial canal/Hunter’s canal). It accompanies the superficial femoral artery in the thigh, initially lateral to the artery then becomes more medial and superior in the distal thigh. Through out its course in the thigh it stays deep to the sartorius muscle. In the leg saphenous nerve is lateral to the saphenous vein and it can be identified either distally near the medial malleolus or at the midcalf.
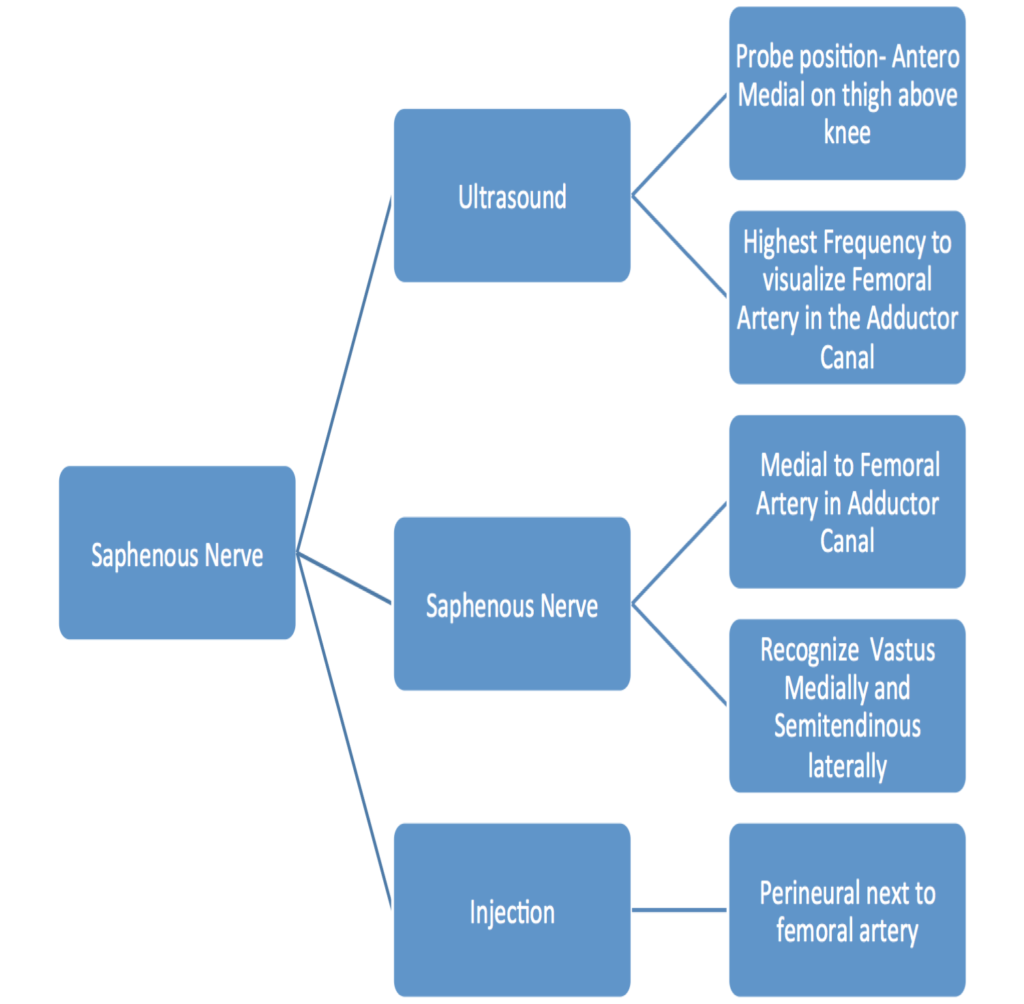

Figure 2
Workflow and anatomy of a saphenous nerve block
Positioning: The patient is placed in the supine position with the leg slightly externally rotated. The medial aspect of the thigh is exposed
Preparation: Clean the injection site in the mid-thightatero-medial area with chlorhexidine or iodine solution.
Equipment: A 22g block needle for single shot or 18 g for catheters. Needles 50mm or 80mm based on the depth of structures.A high-frequency linear ultrasound probe is used.
Technique: The nerve can be easily blocked in the mid-thigh. Both in-plane and out-of-plane approaches can be used. The saphenous nerve is superficial to the femoral artery, deep to the sartorius muscle and posterior to the vastus medialis in the distal thigh. Even in muscular/large BMI population, femoral artery pulsation can be identified Injection of local anesthetic solution anterior to the pulsation (subsartorial injection) provides reliable conduction block.
Complications: Risk of intraneural injection, Local anesthetic systemic toxicity and hematoma at the injection site.
Relative Contraindications: Neuropathy, pre-existing nerve injury/neurological disease.
Absolute Contraindications: Patient refusal, allergy to local anesthetics, and infection or cellulitis at the injection site.
Clinical Pearls: For anterior knee surgery, a more cephalad adductor canal block seems to be more effective in terms of postoperative analgesia. Scan the usual adductor canal landmarks; then slide the probe proximally (upper third of the thigh) and look for the intersection of adductor magnum and sartorius muscles. Perform the block in this point. Recommended LA Volume: 10-15 mL.
Final Recommendation: For the purpose of this case, and for postoperative analgesia of the anterior knee in general, we see the Adductor Canal Block as the most suitable alternative. It offers a reasonable balance between postoperative analgesia and muscle weakness.

Figure 3
Patient and probe position for sephanous nerve block.
Quiz Yourself
We have compiled cases for quick review of ECG and rhythm interpretations for efficient learning and skill enhancement.
