Role of Intraoperative Transesophageal Echocardiography in Guiding Thoracic Endovascular Aortic Aneurysm Repair
Sumeeta Kapoor, MD, Yifan Bu, MD, Benjamin Aronow, MD, Matthew Gao, DO
Published January 23, 2025 | Clinics in Medical Education
Issue 5 | Volume 1 | January 2025
Case 1
A 75-year-old male, 157cm, 51kg underwent thoracic endovascular aortic repair (TEVAR).
Allergy: penicillins (reaction: shaking, has tolerated keflex)
Past Medical History: CABG x4 (2008), HFrEF, LVEF 30% with ICD, PAD (bilateral iliac stents), secondary adrenal insufficiency on prednisone, CKD3, HLD, T2DM, presented with chest/epigastric pain now has penetrating atheromatous ulcer in descending aorta w concern for aortitis
Sugircal History: iliac stent placement bilaterally, penectomy, CABG, bilaterally inguinal lymphadenectomy (2/2 groin infection)
Anesthesia Plans: General Anesthesia with arterial line, central venous line and intraoperative transesophageal echocardiography (TEE).
Case 2
A 83-year-old male with history of atrial fibrillation (no longer on a/c), thoracic aortic aneurysm (TAA) and Aortic stenosis i/s/o biscupid aortic valve s/p aortic valve repair and TAA repair (2014).
The patient was admitted to the BIDMC Vascular Surgery Service via transfer from Cape Cod Hospital with type B aortic dissection w/ proximal descending thoracic aorta diameter 5cm and suspected renal artery malperfusion. The patient underwent left carotid subclavian bypass without complication as stage 1 of surgical treatment plan. Cardiology was consulted for management of atrial fibrillation and blood pressure control. Discharged with carvedilol, amlodipine, and lisinopril in addition to aspirin. Ten days later, the patient was scheduled for thoracic endovascular aortic repair (TEVAR).
Anesthesia Plans: general anesthesia with arterial line, TEE and CVP monitoring for TEVAR.


TEVAR
The use of thoracic endovascular aortic repair (TEVAR) has significantly decreased both morbidity and mortality when compared to traditional open surgical repair. A study utilizing the National Trauma Data Bank revealed a decline in the incidence of open repair, from 7.4% in 2007 to just 1.9% in 2015, while the percentage of TEVAR procedures rose from 12.1% to 25.7% over the same period. TEVAR is also increasingly applied to treat aortic aneurysms, penetrating atheromatous ulcers of the aorta, aortic dissections (type B) and traumatic aortic injuries. As research, clinical interest, and expertise in endovascular techniques have expanded, more advanced and varied procedures have been developed, including chimney TEVAR, and fenestrated and branched TEVAR approaches.
Transesophageal Echocardiography (TEE)
In patients undergoing TEVAR with general anesthesia, TEE provides real-time monitoring of cardiac function, identification of aortic pathologies, guidance for endograft placement, and evaluation of endoleaks after graft deployment. It is also essential for assessing ventricular function and the structure and function of the aortic valve, as thoracic aortic aneurysms (TAAs) and dissections can quickly progress to involve the valve. A comprehensive evaluation of the thoracic aorta is vital to diagnose the primary pathology and detect other conditions such as atheromas. Furthermore, TEE aids in guiding vascular access by visualizing wire placement in the descending aorta. During endograft insertion, it ensures that the aortic pathology is adequately covered. After the graft is deployed, TEE is crucial for confirming that the pathology has been excluded and verifying that no retrograde dissection has occurred. Color Doppler imaging can detect endoleaks but, it may be necessary to reduce the color Doppler aliasing velocity to between 20 and 30 cm per second.
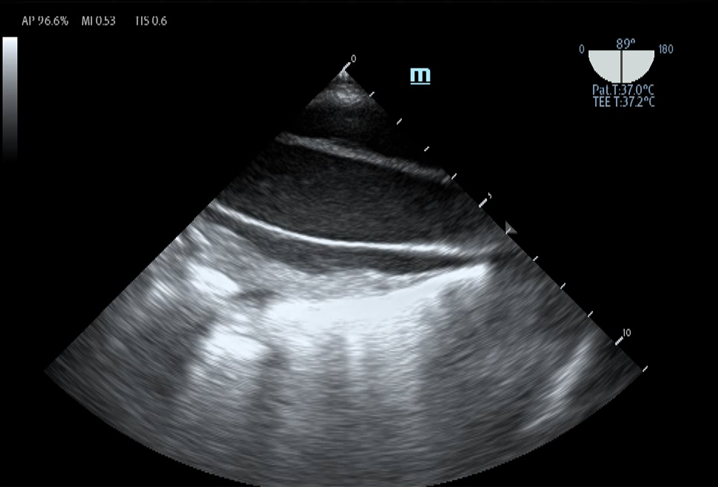
In the first case, pre-procedure TEE identified the descending aorta penetrating ulcer with a size of 0.86×0.55cm and the surrounding intramural hematoma. CFD within the ulcer also appreciated active blood flow, as shown in the TEE image. After the deployment of the stent graft, TEE confirmed the correct apposition of the stent to the ulcer site with no blood flow detected within.
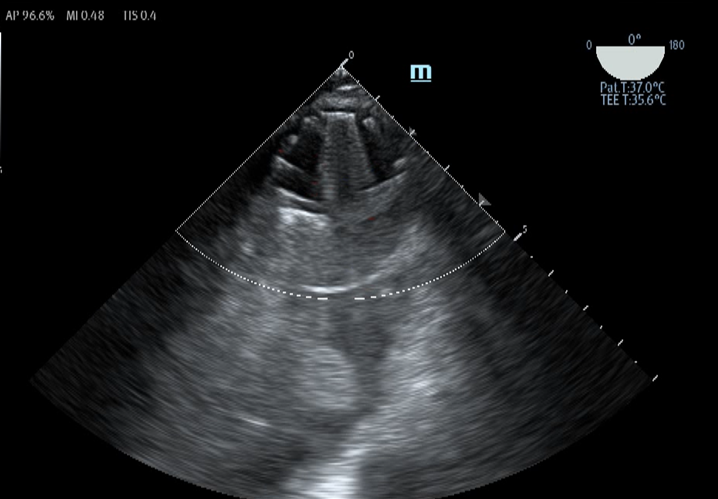
In the second case, pre-procedure TEE was able to further evaluate the complexity of the dissection and the true and false lumen, as shown in the TEE images. After the procedure, TEE showed a full stent deployment without endoleaks and successful exclusion of false lumen with the beginning of thrombosis.
