Optimization of Analgesia for Rib Fractures: Evidence-Based Approaches
Laura Cook, NP, Andrey Rakalin, MD
Published January 23, 2025 | Clinics in Medical Education
Issue 5 | Volume 1 | January 2025
Case 1: Thoracic Epidural
A 78-year-old. male with a past medical history of hyperlipidemia, asthma, multiple cerebral cavernous malformations s/p R cerebellar cavernous malformation resection (2014), chronic kidney disease presented with mechanical fall from bed four days ago. He was found to have displaced left 9-11th rib fractures and right 11th rib fracture.
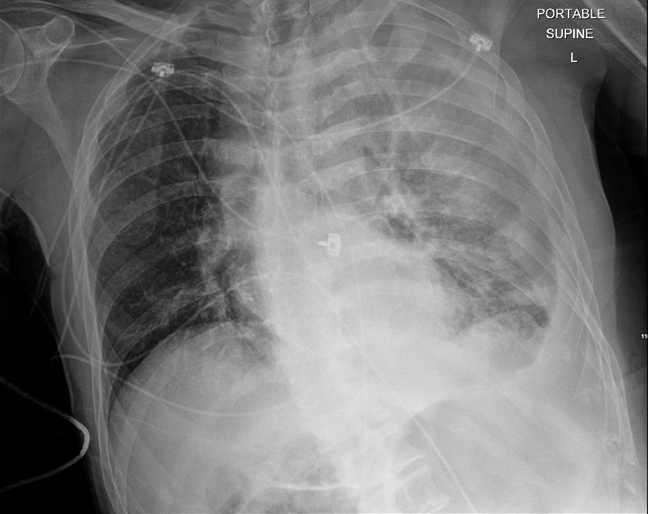
Chest x ray Day 1: Minor basilar atelectasis is seen without focal consolidation. No pleural effusion or pneumothorax is seen. The cardiac and mediastinal silhouettes are stable; mediastinal contours are similar compared to previous xray. The aorta may be tortuous.

Day 2
He became tachypneic and hyoxic with RR 24 and the chest xray showed left chest wall hematoma c/b intercostal artery pseudoaneurysm. A left chest tube was placed. An epidural catheter was placed at T8/T9 for post-traumatic analgesia management.
Chest x ray: New filamentous tubing projects over the lower midline chest, possibly for administering spinal anesthesia. The large bore left thoracostomy tube is in position ascending along the midline. Very small left apical pneumothorax and the small, residual left hemothorax is stable. Large scale consolidation at the base of the left lung, probably atelectasis, and substantial subsegmental atelectasis worsened at the base of the right lung, could both be contributing to hypoxia. Mild interstitial edema persists, left greater than right. Displaced bilateral lower rib fractures are shown.
The following multimodal approach was recommended for this patient:
1. Post-operative analgesia recommendations: Epidural Analgesia: (1) Bupivacaine 0.1%-Hydromorphone 10mcg/mL @ 4-12 mL/hour; rate 10 cc/hr, (2) Naloxone 100-200 mcg/hr (5-10 mL/hr) IV continuous PRN -if needed for pruritus only. (3) Acetaminophen 1gm IV q6H Systemic Anticoagulation was contraindicated while epidural in place due to heightened risk of epidural hematoma
2. VTE Prophylaxis: SC heparin must be limited to <15,000 units/day with coagulation monitoring on day of removal or placement. 10,000 units per day is preferential or Enoxaparin 40mg SC daily (<1mg/kg daily). Delay anticoagulation the morning of planned catheter removal. Following neuraxial catheter removal, delay administration of SC heparin 1 hour or enoxaparin 4 hours. Venodyne boots while sedentary
3. Urinary retention: Urinary catheter is required based off neuraxial catheter location in the lumbar or low thoracic spine (T9,T10,T11) due to an increased risk of urinary retention. Remove immediately following epidural removal. No IUC is required based off epidural placement.
On day 5, the patient stabilized and the catheter was removed.
Case 2 : Ultrasound guided parasternal block and Pectoralis 2 Block
A 71-year-old man with type 1 diabetes mellitus with retinopathy, neuropathy and CKD, HTN. HFrEF (EF 40%, most likely ischemic) who presented initially with dyspnea and cough, volume overload (decompensated HF), course c/b torsades and cardiac arrest s/p ROSC, was transferred to CCU for management. He has had good recovery from his arrest but has chest discomfort related to rib fractures and was managed on oxycodone.
CT report: Nondisplaced fractures in the right anterolateral 2-6 ribs and left anterolateral 2-4 ribs.
Moderate bilateral nonhemorrhagic pleural effusions, right greater than left, accompanied by substantial relaxation atelectasis in the lower lobes. Superimposed pneumonia can not be excluded, especially in light of subtle peribronchial infiltration in both lower lobes and posterior segment of the left upper lobe.
Acute pain service was consulted and performed an ultrasound guided parasternal and PEC 2 block on the right.
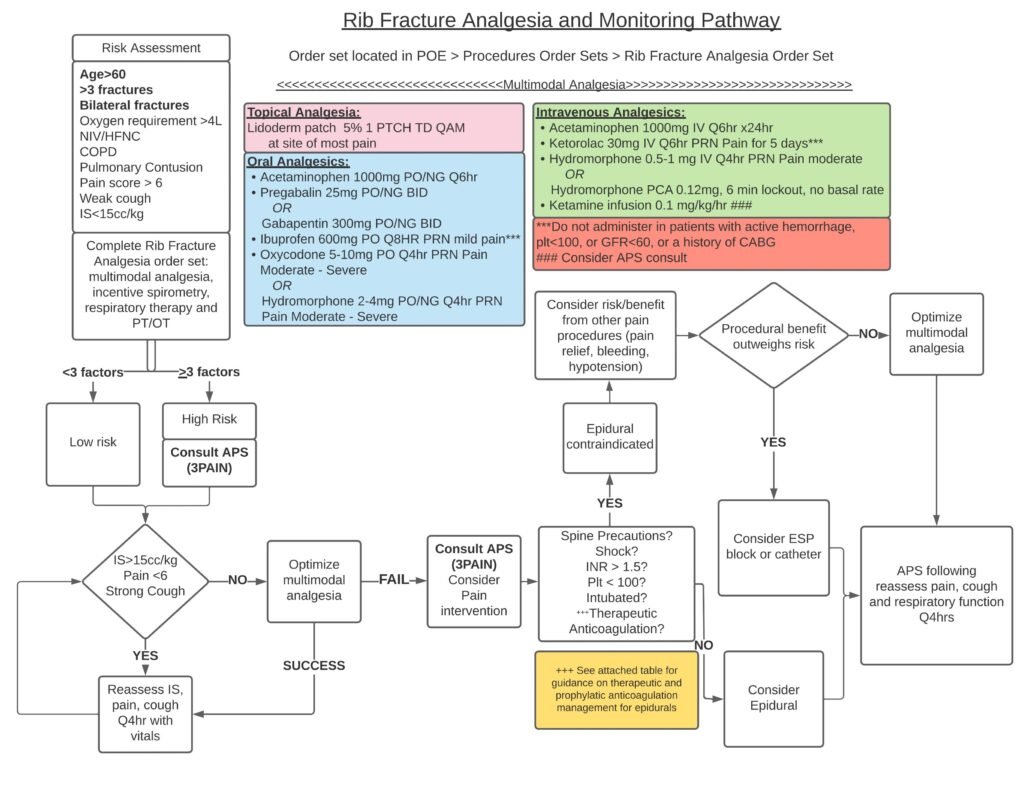
The protocol for rib fracture analgesia is shown below.