Advancing Clinical Ultrasound Education: Recognizing the Need for Credentialing and Privileges in Anesthesiology
Robina Matyal, MD
Published April 18, 2025 | Clinics in Medical Education
Issue 6 | Volume 1 | April 2025
Ultrasound is no longer a diagnostic luxury—it has become a procedural essential in anesthesiology, critical for tasks such as vascular access, nerve blocks, and cardiac assessments, where it enhances precision, safety, and efficiency. Recognizing its importance, the American Board of Anesthesiology (ABA) requires trainees to attain Level 4 and 5 competency in ultrasound-guided procedures. However, many institutions struggle to meet this standard due to a shortage of trained faculty, which limits opportunities for hands-on instruction and mentorship. Addressing this gap requires a dual approach: individual responsibility, where practitioners take initiative to achieve proficiency, and institutional responsibility, where departments provide structured, curriculum-based training led by qualified faculty. Together, these elements form the foundation for effective credentialing and privileging, ensuring the safe and consistent use of ultrasound in clinical care.
Individual Responsibility in Clinical Ultrasound Training
Individual physicians carry the responsibility to actively engage in training, seek feedback, and demonstrate ongoing competency. Mastery of Clinical Ultrasound requires continuous learning and self-assessment to ensure safe, effective practice. Credentialing should reflect not only completion of training but also a clinician’s personal commitment to maintaining proficiency in this evolving skill.

Institutional Responsibility in Clinical Ultrasound Training
Clinical Ultrasound is increasingly recognized as a valuable tool in anesthesiology, enhancing diagnostic accuracy and guiding clinical decision-making. However, a critical challenge remains: how should anesthesiologists be trained, assessed, and credentialed in this evolving technology? The Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Anesthesiology (ABA) have recognized ultrasound-guided techniques as essential training milestones since 2013. Despite this, there is no standardized curriculum for practicing anesthesiologists, leading to significant variability in proficiency. This gap highlights the responsibility of institutions and departments to ensure comprehensive ultrasound education through structured, competency-based training rather than relying solely on certification. A proactive, structured approach—combining didactics, hands-on training, and standardized assessments—is essential to bridge the ultrasound proficiency gap. Institutionalizing such training ensures anesthesiologists meet the evolving demands of modern practice with consistency and quality.
Certification vs. Proficiency in Clinical Ultrasound Training
The adoption of new medical technologies often outpaces formal training guidelines. This has been observed in laparoscopic and robotic surgery, where a bottom-up approach led to structured proficiency pathways. Conversely, transesophageal echocardiography (TEE) followed a top-down model, emphasizing certification without necessarily ensuring hands-on proficiency.
A top-down approach to perioperative ultrasound would define certification as the goal without outlining a structured pathway to proficiency. This model identifies experts but does not necessarily build widespread competency. A bottom-up approach, on the other hand, focuses on developing practice pathways that enhance knowledge and grassroots familiarity, ultimately defining proficiency as the goal.
Currently, clinical ultrasound training lacks a standardized approach, particularly for practicing anesthesiologists. While trainees and students are increasingly exposed to ultrasound techniques, those already in practice often lack a formalized curriculum. This raises an important question: Should the field prioritize certification or focus on demonstrated competency for credentialing?
A Model for Clinical Ultrasound Training and Credentialing
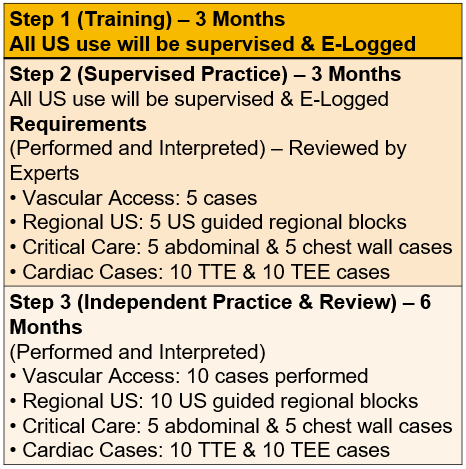
At Beth Israel Deaconess Medical Center (BIDMC), a structured curriculum has been developed to bridge this gap. This program includes:
- Didactic Sessions
- Online Self-Training Tool
- Workshops (5-6 per year) and Case-Based Discussions
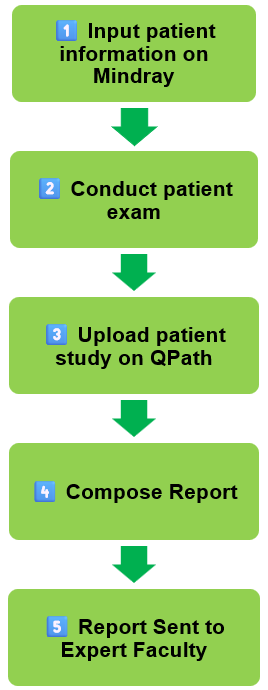
However, training alone is insufficient. A comprehensive system for quality assurance, credentialing, and billing must accompany educational initiatives. BIDMC addresses this by utilizing Qpath, a cloudbased, HIPAA-compliant software that securely stores images and reports for review, ensuring standardized quality control and facilitating billing for Clinical Ultrasound exams.
Moving Forward: Establishing a Path to Recognition
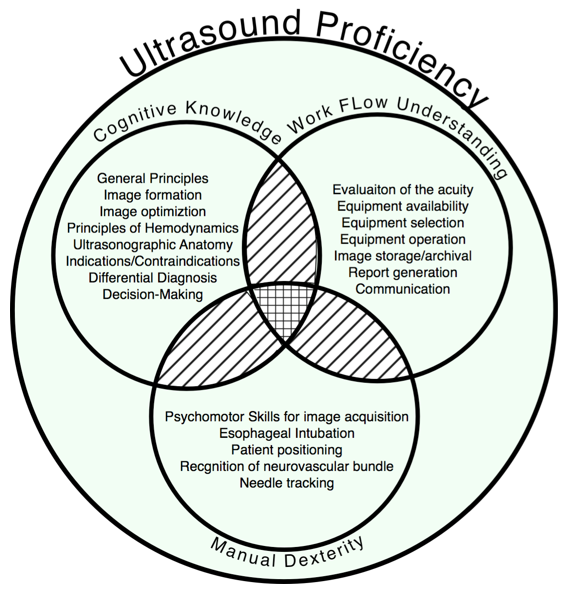
Rather than pursuing certification as an endpoint, the focus for Clinical Ultrasound training should be on demonstrated competency. For anesthesiologists to obtain hospital-based privileges and credentialing, they must be able to consistently display clinical proficiency. Departments must take ownership by providing a comprehensive, curriculum-based training program that emphasizes both cognitive understanding and manual dexterity. This should be coupled with ongoing competency evaluations, image review, and supervised clinical application.
Institutions also bear the responsibility of establishing a robust quality assurance system that supports continuous skill development and ensures high standards in clinical practice. By investing in structured training and formalized pathways for credentialing based on performance, departments can move beyond the limitations of certification and toward meaningful recognition that directly supports patient safety and clinical excellence.
