Implementing Virtual Reality in Procedural Training Curriculums: Using Technology to Improve Clinical Training and Proficiency
Shiri Savir, MD (Moderator), Robina Matyal, MD (Panelist), Sara Neves, MD (Panelist), John Mitchell, MD (Panelist)
Published April 18, 2025 | Clinics in Medical Education
Issue 6 | Volume 1 | April 2025
At the 2025 IARS Annual Meeting, the session “Stepping Into the Future: Implementing Virtual Reality in Invasive Procedural Training Curriculums” featured expert panelists who shared forward-thinking strategies for integrating VR into procedural education.
Why Immersive Training Matters for Anesthesia Education
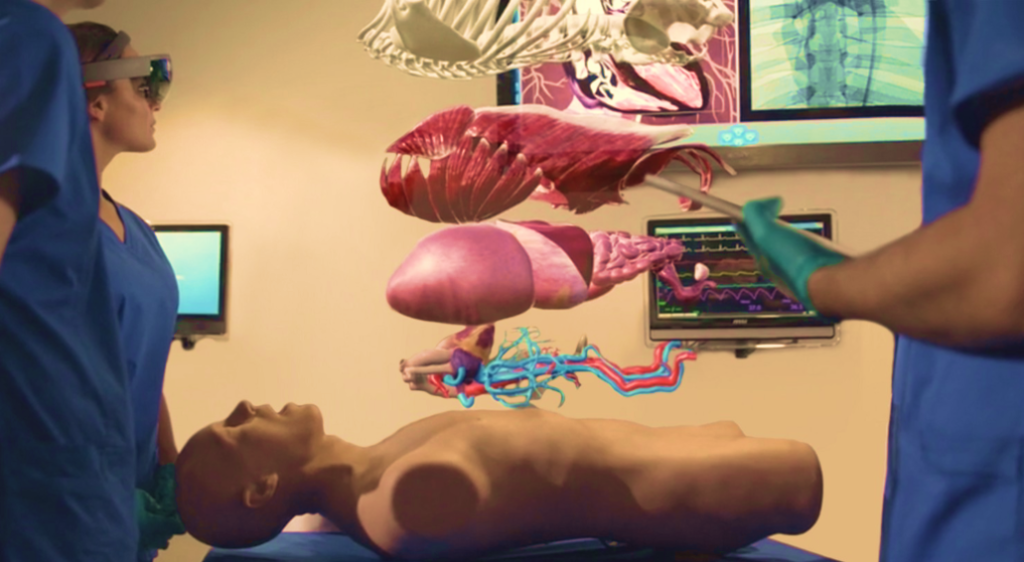
Anesthesia is a high-stakes specialty requiring rapid decision-making and technical precision, often in life-threatening situations. Traditional training methods, such as lectures and protocol reviews, do not fully prepare trainees for real-world emergencies. Immersive technologies, including virtual reality (VR), augmented reality (AR), in situ simulations, and Artifical Intelligence-powered ultrasound are transforming anesthesia education by recreating high-pressure clinical scenarios in a controlled, interactive environment.
Research shows that simulated crisis exposure enhances performance, strengthening both technical and cognitive skills. For example, repeated simulation of rare but critical emergencies, such as a “cannot intubate, cannot ventilate” scenario, build muscle memory and rapid-response capabilities. These advanced training modalities provide real-time feedback, reinforce critical thinking, and cultivate teamwork, ensuring that anesthesia providers respond to high-stress situations with well-practiced, lifesaving interventions.
Limitations of Traditional Anesthesia Training
The current model for procedural skills training is largely apprenticeship-based, where learning depends on clinical exposure, case volume, and instructor availability. However, this model presents several challenges:
- Inconsistent learning experiences due to variations in training environments (university vs. community hospitals).
- Limited hands-on opportunities because of clinical workload priorities.
- Patchy exposure to complex cases, leading to variable proficiency levels.
- Difficulty assessing manual dexterity where proficiency is often assumed rather than objectively measured.
A curriculum-based approach, integrating task training with cognitive learning, has been shown to improve skill acquisition and transferability to clinical practice. Surgical residents trained using structured simulation programs demonstrate greater clinical competence and confidence compared to those relying solely on traditional models.

Augmented and Virtual Reality: The Future of Procedural Training
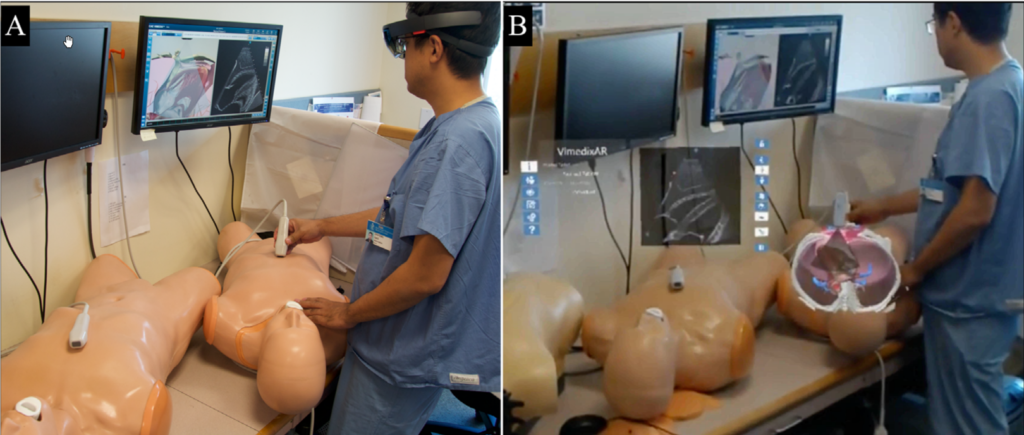
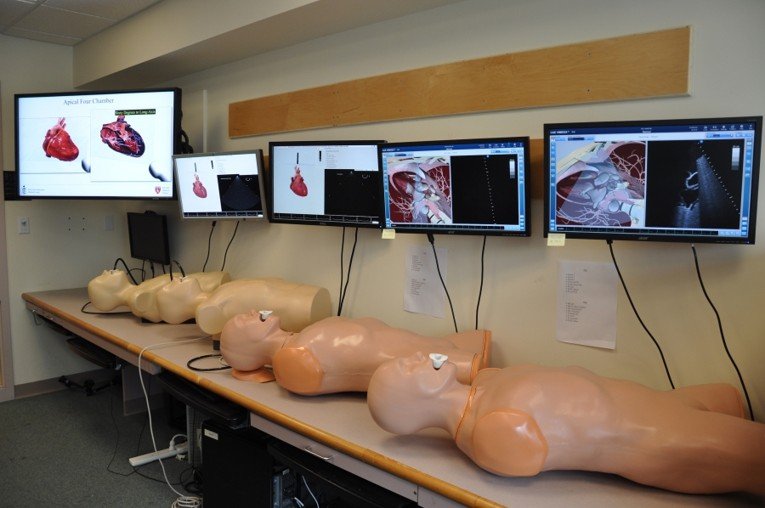
Augmented Reality (AR) Simulation
- Enhances realism and spatial understanding of anatomical structures.
- Allows real-time feedback, error detection, and collaborative learning.
- Easily integrates with existing simulation tools.
- Challenges: Complex setup, faculty training needs, and cost considerations.
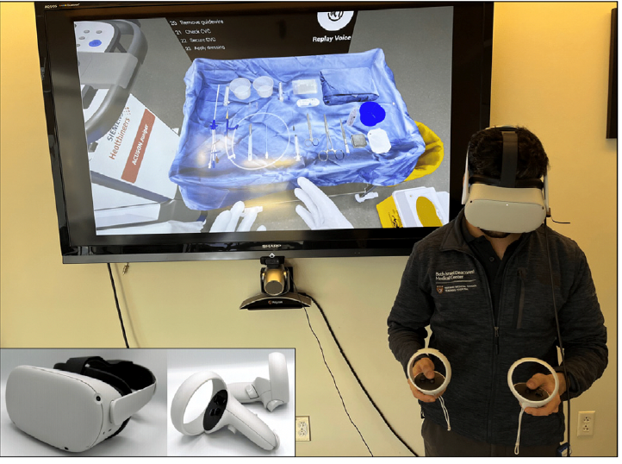
Virtual Reality (VR) Simulation
- Provides highly realistic, hands-on practice with immediate feedback.
- Tracks performance, enhances retention, and boosts trainee confidence.
- Cost-effective, portable, and scalable for widespread use.
- Challenges: Limited haptic feedback, faculty adaptation issues, and difficulty replicating patient interactions.

Moving Forward: A Structured Approach to Training and Credentialing
To maximize the benefits of immersive training, institutions must adopt structured curricula that balance cognitive learning with hands-on skill acquisition. Incorporating VR and AR into anesthesia education will not only reduce the learning curve but also improve patient safety and procedural efficiency. By shifting from traditional apprenticeship models to evidence-based, technology-driven training, we can create pre-trained experts rather than pre-trained novices, ensuring anesthesia providers are proficient, confident, and prepared for real-world clinical challenges.
